Lancet Glob Health. 2025 Apr;13(4):e707-e715. doi: 10.1016/S2214-109X(24)00527-8.
ABSTRACT
BACKGROUND: Secondary antibiotic prophylaxis is the only intervention known to prevent rheumatic heart disease progression, yet delivery of prophylaxis at scale in low-resource settings has proven challenging, undermining many global programmes. We sought to assess whether enhanced prophylaxis support for rheumatic heart disease, administered through community health workers in the public health system, was feasible and a scalable model.
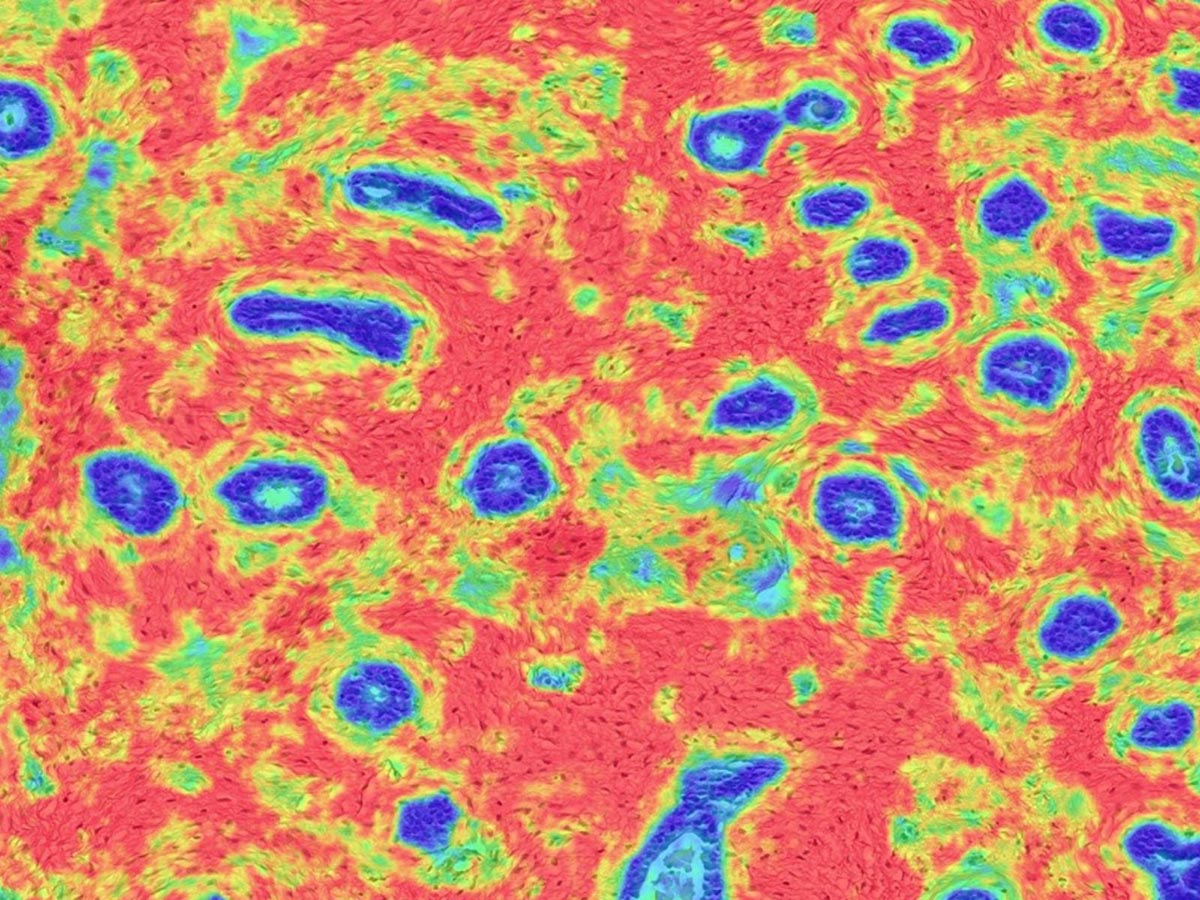
METHODS: The CAMPS trial was a pragmatic randomised trial of prophylaxis supports integrated into routine care in Eastern Uganda. Children and adolescents with rheumatic heart disease who were aged 5-17 years were randomly assigned (1:1) using permuted block randomisation to either usual care or enhanced support. Enhanced support consisted of case managers and peer groups. Participants and providers were not masked to treatment assignment due to the study design. Children were followed up for 12 months to compare the primary outcome of prophylaxis adherence, measured as a continuous variable of days covered, using a modified intention-to-treat analysis principle. Secondary outcomes were treatment satisfaction, and patient and caregiver health-related quality of life scores. This trial is registered at ClinicalTrials.gov, NCT05502042, and has been completed.
FINDINGS: Between Aug 9, 2022, and Aug 9, 2023, 208 individuals were enrolled in the study and included in the analysis. 104 (50%) individuals were randomly assigned to the usual care group and 105 (50%) to the enhanced support group; one participant in the usual care group was excluded from the primary analysis as they died before the first injection, meaning that 103 participants were analysed in the usual care group. 121 (58%) participants were female and 87 (42%) were male. After 12 months, mean adherence was 80·0% (SD 19·0) for those receiving usual care, compared with 98·2% (7·1) for those receiving enhanced support (estimated mean difference in adherence of 18·2%, 95% CI 14·4-22·1; p<0·0001). No significant differences were found between groups in treatment satisfaction (mean between-group difference of 0·1 points [95% CI -1·9 to 2·1] at 12 months) or quality of life (2·3 [-1·1 to 5·8] for patient score; 1·3 [-1·6 to 4·1] for caregiver score).
INTERPRETATION: The integration of community health workers into rheumatic heart disease supports within the public health system provides an effective and likely scalable model to improve outcomes for children with rheumatic heart disease in low-resource settings. Further research should examine scale-up and scale-out of these strategies, formally explore cost, and rigorously partner with diverse groups of patients to shape adaptations to this design and ensure appropriateness for all groups affected by rheumatic heart disease.
FUNDING: Thrasher Research Fund Early Career Award and Edwards LifeSciences Foundation.
PMID:40155108 | DOI:10.1016/S2214-109X(24)00527-8
Authors: Sarah de Loizaga, Jafesi Pulle, Okumu Atanas, Juliet Alepere, Jane-Liz Nambogo, Emma Ndagire, Gloria Kaudha, Nicholas J Ollberding, Emmy Okello, Joselyn Rwebembera, Andrea Beaton
Published: 2025-03-28 10:00:00
Read the full article: View on PubMed